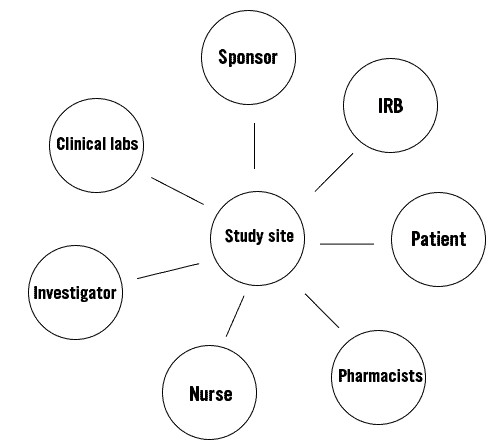
The sponsor of a study will assign one or multiple principle investigators (PI), usually a doctor. Along with a team of nurses and other stakeholders, the PI will conduct the trial at his/her study site. However, the sponsor will remain the monitor of the trial. The next figure shows the important stakeholders in a clinical trial.
Traditionally, clinical trials have never been designed with patient-centricity in mind. Although the patient has always been part of a trial as a human subject, they were never really considered an important stakeholder. Communication and engagement are low, and the patient only comes into the picture during the recruitment phase.
It is a well-known fact that the costs related to clinical trials are taking up a large amount (up to 90%) of the total R&D costs. This combined with the rising complexity of clinical trial, leads to development times of 10-12 years per drug on average and ridiculously high medication costs for patients. Not only is this inconvenient, according to some experts, it kills on average 35,000 patients who are waiting on potentially live saving drugs to move through the clinical trial process. Although there are initiatives, such as fast-track-life-saving drugs, to shorten the lab to patient time, fundamental changes in the rigor of the procedure of clinical trials are mandatory.
Patient-centric clinical trial design
Over the years, an increase in competition within the drug development industry and the complexity of products and protocols, has led to a search for new strategies with the aim of being more efficient, having a higher patient engagement and speeding up the study timelines. In 2015, a survey showed that 75% of all clinical trial professionals interviewed (n=427), reported putting the patient at the heart of the trial as their top priority. Furthermore, they identified enrolment speed (42%), narrowing patient eligibility criteria (23%) and patient retention (20%) as their biggest challenges.
The general idea of patient-centric research is to make a shift from solely focussing on the efficacy and the convenience of the researcher, to a design focussed on the needs and convenience of the patient. The patient should not just be a human subject, but an engaged stakeholder. Only limiting patient-centricity to the execution of a trial, would be counter-intuitive, as they are the reason to produce new treatments and from a practical point of view, can help with understanding how to find patients and keep them engaged.
It is inevitable that clinical research requires a bit of extra effort from the patients, but patient-centric trials focus on making the participant work smarter, not harder, while still being able to reap the benefits. There are many different ways to make a trial more patient-centric, such as:
- recruiting patients through social media
- study branded schedules and guides designed to educate and inform the patient
- reporting through applications
- online informed consent
- open communication
- data transparency
- patient-centred outcomes
- video conferencing
- …
One other way to make a trial more patient-centric, is to bring the trial to the patient instead of the patient to the trial through the implementation of home visits.
Contact us today and discover all the benefits of Home Trail Support.
